Mental illness diagnosis in young adults faces challenges due to subjective assessments, symptom overlap, and limited understanding of individual experiences, leading to high misdiagnosis rates. Despite effective therapies like Cognitive Behavioral Therapy (CBT), improved diagnostic tools are needed. Crisis intervention, resilience building, and burnout prevention for healthcare providers are crucial areas to enhance accuracy and tailor therapy plans for young adults struggling with mental health issues. Public awareness campaigns destigmatizing mental illness also encourage early help-seeking.
Mental illness diagnosis accuracy is a critical aspect of healthcare that significantly impacts patient outcomes, particularly among young adults. Despite advancements, challenges remain in identifying and treating mental health conditions, leading to misdiagnosis and delayed treatment. This article explores the current state of mental illness diagnosis, its limitations, and the potential for improvement. We delve into Cognitive Behavioral Therapy (CBT) as an effective tool for enhancing diagnostic precision and discuss innovative approaches, including technology integration and collaborative care models, paving the way for more accurate and timely interventions, especially for young adults seeking therapy.
- The Current State of Mental Illness Diagnosis: Challenges and Gaps
- – Exploring the limitations of current diagnostic methods
- – Prevalence of misdiagnosis and its impact on young adults
The Current State of Mental Illness Diagnosis: Challenges and Gaps

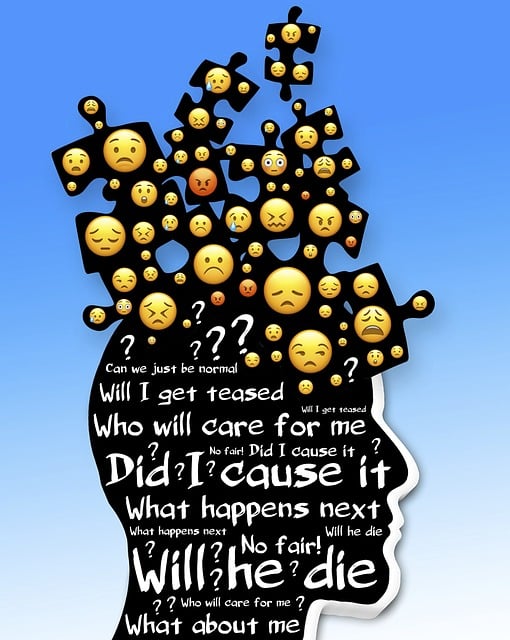
The current state of mental illness diagnosis faces several challenges and gaps, hindering effective treatment and support for individuals suffering from various conditions. Despite significant advancements in understanding mental health, diagnoses often lack precision, leading to misinformed care plans. The complexity of human emotions and behaviors makes it difficult to pinpoint specific disorders, especially when symptoms overlap. This is particularly true for young adults who may present with unique expressions of distress, making diagnosis even more intricate. For instance, what appears as anxiety in one person could be a manifestation of depression in another, requiring nuanced approaches.
Cognitive Behavioral Therapy (CBT) stands out as a prominent therapeutic approach, yet its application is not without limitations. While CBT has proven effective for many, especially in managing anxiety and depression, it may not address the underlying complexities of certain mental health conditions. Crisis intervention guidance, resilience building, and burnout prevention are crucial aspects that demand attention to bridge these gaps. Enhancing diagnostic tools and techniques will foster more accurate evaluations, enabling tailored therapy approaches and ultimately improving outcomes for young adults navigating their mental health journeys.
– Exploring the limitations of current diagnostic methods

The current diagnostic methods for mental illness often fall short due to their reliance on subjective assessments and limited understanding of individual experiences. Traditional approaches, such as structured interviews and standardized questionnaires, while valuable, can be imprecise in capturing the complex nature of mental health conditions. These tools may not adequately account for cultural differences, personal interpretations, or the unique presentation of symptoms in diverse populations. As a result, diagnoses can sometimes be inaccurate or delayed, leading to suboptimal treatment outcomes.
For young adults, this is particularly concerning as they navigate their identity and independence. Cognitive Behavioral Therapy (CBT), a widely recognized therapy for mental health issues, has shown promise in improving diagnostic accuracy. CBT helps individuals identify and challenge negative thought patterns, fostering resilience building and better mood management. Moreover, public awareness campaigns focused on destigmatizing mental illness can encourage young adults to seek help earlier, enabling more effective interventions and supporting their overall well-being.
– Prevalence of misdiagnosis and its impact on young adults

The accuracy of mental illness diagnoses is a pressing issue, especially for young adults. Studies show that misdiagnosis rates are alarmingly high, with up to 30% of cases incorrectly identified on first assessment. This has significant consequences for this vulnerable demographic, often leading to inappropriate or delayed treatment. Young adults who receive an incorrect diagnosis may undergo unnecessary and potentially harmful interventions, while those with genuine mental health conditions might not access the right support due to diagnostic errors.
Imprecise diagnoses can foster a cycle of frustration and mistrust between patients and healthcare providers. It impacts the effectiveness of therapy for young adults, particularly when treating complex cases that involve comorbidities or subtle symptoms. Cognitive Behavioral Therapy (CBT), alongside Mindfulness Meditation and Self-Awareness Exercises, has gained recognition as effective interventions. However, to enhance diagnosis accuracy, Burnout Prevention Strategies for Healthcare Providers are essential. These strategies ensure professionals remain alert, objective, and adept at recognizing the nuances of mental health presentations in young adults.
Mental illness diagnosis accuracy is a critical aspect of patient care, especially for young adults. By recognizing the challenges and gaps in current methods, such as misdiagnosis rates, we can make significant strides forward. Integrating evidence-based practices like Cognitive Behavioral Therapy (CBT) offers promising solutions to enhance diagnostic precision. Through continued research, education, and access to specialized therapy for young adults, we can improve overall mental health outcomes and ensure individuals receive the appropriate support they need.